Binghamton researchers developing muscular dystrophy drug
MD drug development is measured in years, dollars and luck
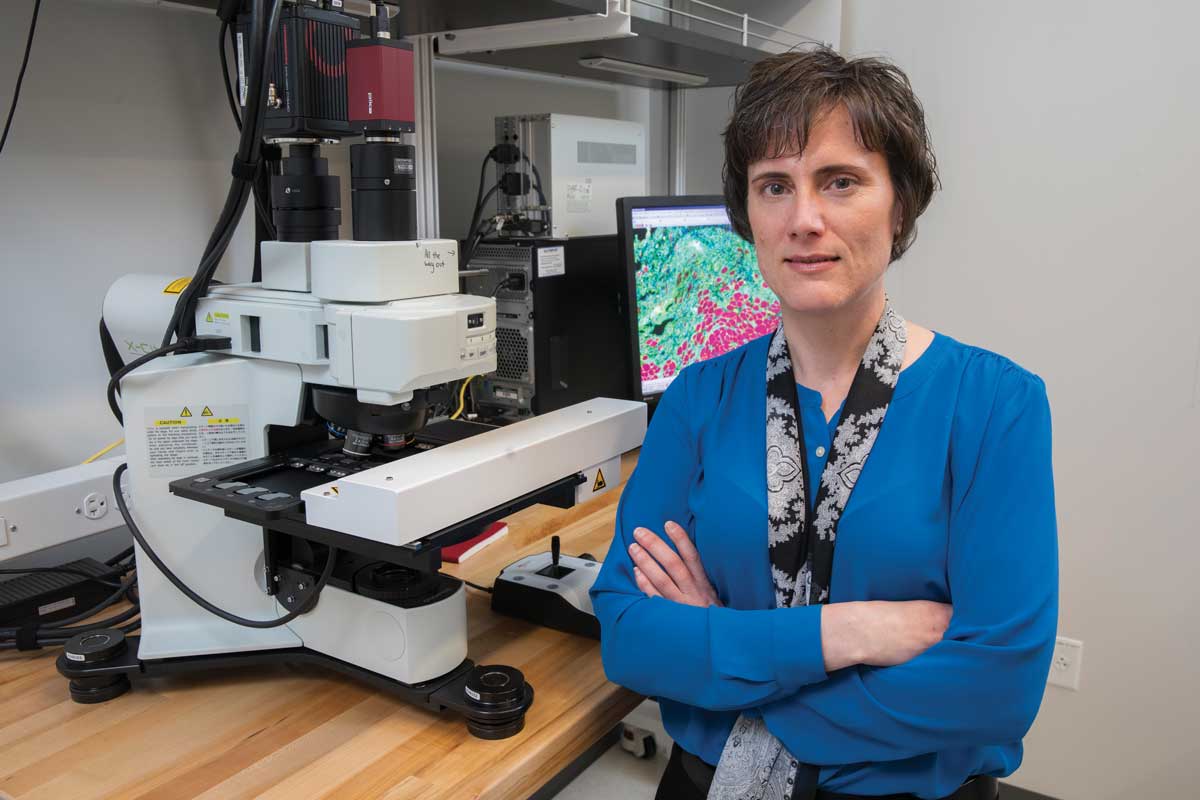
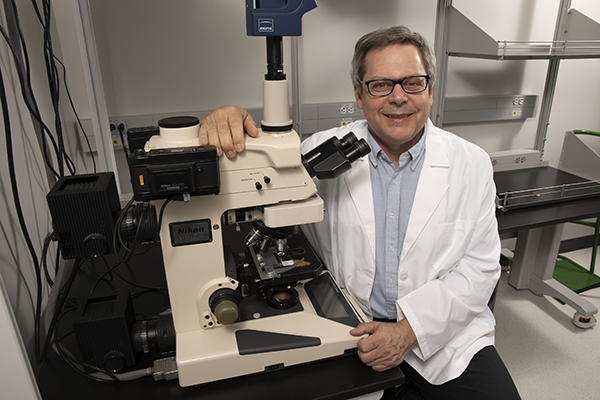
When Kanneboyina Nagaraju, professor and chair of Binghamton University’s Department of Pharmaceutical Sciences, and Eric Hoffman, associate dean for research at the School of Pharmacy and Pharmaceutical Sciences, set out to find a drug to treat patients with Duchenne muscular dystrophy (DMD), a rare genetic disorder that presents itself in children between the ages of 3 and 5, they knew it was a long shot. The pair had been working on translational research together for 20 years before coming to Binghamton in 2016 and knew the challenges.
It was a long shot not because of the condition itself — the cause of the disease was already well known. But instead, it had to do with drug development, which takes decades and tens of thousands — even hundreds of thousands — of failures along the way, not to mention millions of dollars in funding. And that’s if you’re lucky enough to find a compound that both works and is not harmful to people.
Add the further complication that most pharmaceutical companies aren’t going to fund a drug for a rare disease, and it’s an uphill climb.
“We’re looking for needles in a haystack,” says L. Nathan Tumey, assistant professor of pharmaceutical sciences, who was a leader in multiple drug-discovery programs during his years in the pharmaceutical industry. “Out of maybe 100,000 compounds, we might pull out 20 that interact with the target.” And of those 20, maybe one — or none — will have properties suitable for initiating a drug-discovery program. Here’s what it takes to thread the needle once it’s found.
Where to start
The first step in drug design is knowing what goes wrong to cause the disease, whether it’s a specific mutated protein, DNA sequence or signaling pathway that goes awry. That becomes the target.
DMD, for example, is caused by the absence of dystrophin, which plays an important role in muscle repair. Normally when a muscle is stressed (like when you lift weights or run), that muscle is slightly damaged. Dystrophin is a protein that helps heal the muscle and keeps muscle cells intact.
Children with DMD don’t make dystrophin, so the muscle is continually undergoing damage but has increasing trouble repairing itself. These children become less mobile as they age. They are typically wheelchair-bound in their teens and only live into their early 20s. “It’s a 100% lethal disease,” Nagaraju says. A drug therapy for DMD would address the lack of dystrophin.
Once the biology of the disease is understood, the next step is to identify a “lead compound” that can spur change in the underlying disease progression. That can be done in three ways, Tumey said. The first is to screen libraries for possible compounds to identify ones that interact with the biological target of interest.
“We have collections of potential drug molecules in the range of 100,000 to 500,000,” he says. “We use robotics and high-throughput methods to screen them one by one by one.”
The second is rational design, where researchers take what they know about the problem on a molecular level and use computer modeling to design molecules they think would work. Synthetic chemists then go into the lab to build and test them — thus making the leap from theory to reality.
The third is when researchers stumble upon a treatment, but they don’t exactly know what’s driving the effect. A well-known example, Tumey said, is the ancient remedy of chewing on willow bark to reduce fevers and alleviate pain. Researchers worked backward with that knowledge and developed aspirin.
A more modern example involves an extract from the bark of the Pacific yew tree. Scientists knew that the extracts had interesting anticancer properties, but initially did not know the specific component that drove this effect. Many years of studies in academic labs, in government research labs and in the pharmaceutical industry led to the development of taxol — a highly effective treatment for a variety of cancers.
Bracing for failure
While 100,000 to 500,000 potential drug molecules to screen might seem like a bounty of options, the majority are going to fail before they are ever tested in a disease model. Even then, most will not make it past testing in animal models.
“The body is so complicated,” says Aaron Beedle, associate professor of pharmaceutical sciences. “Many of those ideas, even though they seem really good, do not pan out.”
Drugs fail for a lot of reasons: Perhaps the drug works against the condition but can’t be targeted at just one place and causes problems when the entire body is exposed instead; or the side effects do more harm than good. Most often, though, she says, “There’s something we don’t know yet, or it interacts in some way that we don’t understand.”
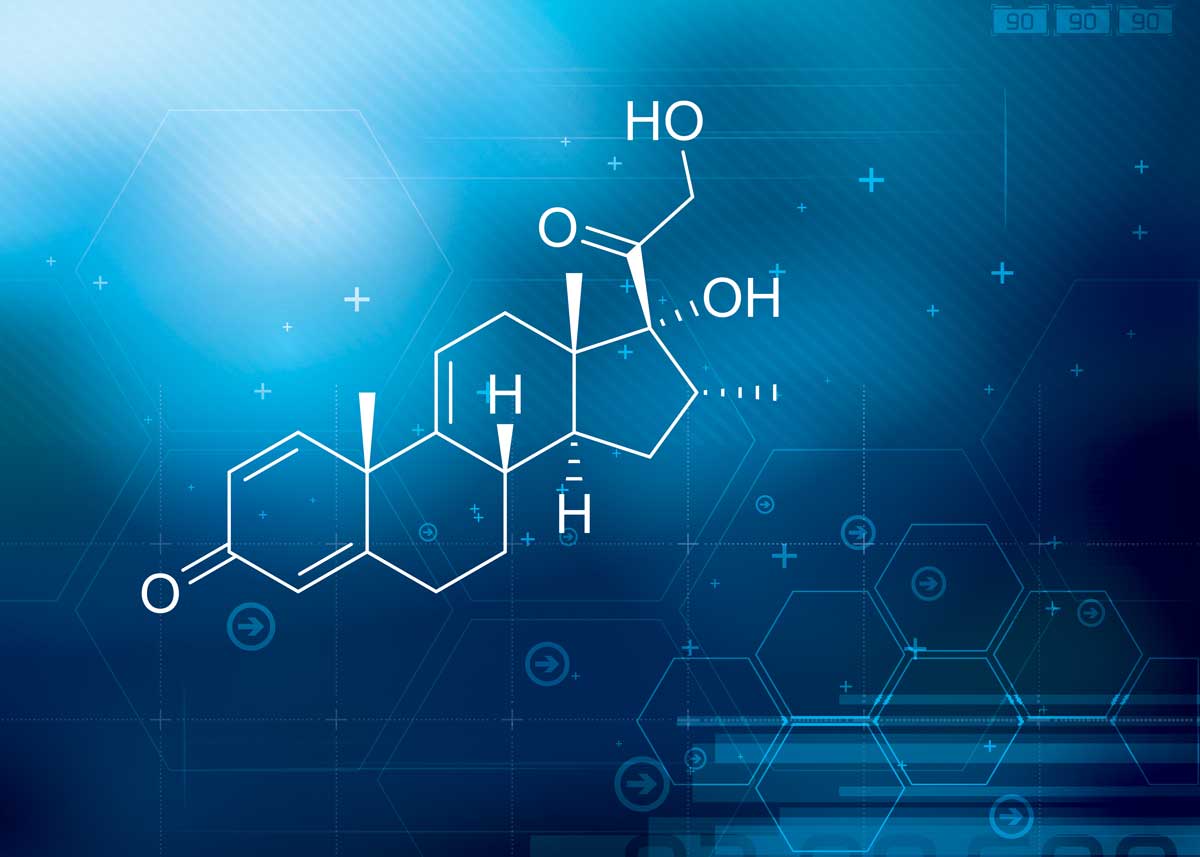
The current treatment for DMD is the steroid prednisone, which improves muscle strength and function but with severe side effects, including weight gain, behavioral changes and high blood pressure. But a new drug developed by Nagaraju and Hoffman, called vamorolone, is showing promise as an alternative. It binds to the same receptors as prednisone, but doesn’t have such harsh side effects.
The compound that worked was the 15th drug they screened. That’s why, in order to make drugs, you must be comfortable with failure, Nagaraju says. It didn’t get him down all that much because, he said, there’s already an “enormous amount of failure” that goes with being a researcher.
“Ninety-three percent of the grants I applied for failed,” he says. But the 7% success rate still meant 7% were funded. It also helps to have the end goal in mind.
“What’s kept us going is not the money, but hopefully I can sleep well one day knowing we did something good for these kids,” he says.
Beedle says it’s also something that they get used to over time. “When we publish papers, everything we put out is being critiqued and accepted or denied. More grant applications are denied than are ever accepted,” she says. “In order to even make it in this field, we have to have some sort of innate ability to survive withstanding failure.”
Testing in stages
To get to clinical trials in humans, drugs have to go through several steps, including testing in animal models. Preclinical toxicology testing must show the drug is safe before clinical trials can be initiated.
All of these steps leading up to trying drugs in people is not a bad thing, Beedle says. That’s because she wants to know as early as possible that a drug is either not safe for patients or not going to work. That’s important in making sure that children and their parents don’t build up expectations that can’t be met.
“Every single time a patient gets enrolled in a clinical trial, that’s the family’s best hope. I don’t think anything should be going to clinical trial until we are absolutely as confident as we can be about its potential,” she says. “To put patients into trials and have them fail is really heartbreaking. I wouldn’t want anything out there that I didn’t have as much confidence in as I possibly could.”
Once clinical trials in humans are approved, researchers move slowly, in steps. In the case of vamorolone, its phase I trial tested the drug’s safety on 86 healthy adult men in 2015. In the next three series of trials, the drug was tested on 48 boys with DMD, and an additional trial of 120 boys began in August 2018.
Nagaraju and Hoffman attended a European Medicines Agency meeting this past summer to see if they have enough data showing the drug’s efficacy and safety for approvals in Europe. Their final trials are expected to finish next year, and they expect to go to the FDA for approval in the United States in fall 2020.
Funding the research
Most drug research is paid for by the National Institutes of Health and the pharmaceutical industry, Hoffman says. Venture capitalists also look for promising drugs for what most consider high-risk investment because of the high failure rate — but also the potential for a big reward.
“The assumption is that most venture capitalists go into drug development for at least 10-fold back on their investment,” he says. “If they can’t get that, they aren’t going to invest.”
DMD affects approximately one in every 3,500 male births. It’s a so-called orphan disease, one that affects fewer than 200,000 people nationwide. Because of that status, drugs to treat it are never going to garner much attention from pharmaceutical companies or venture capitalists.
“If the disease affects a handful of people, nobody wants to put out the money because it doesn’t make business sense,” Nagaraju says. “But pain and suffering are the same whether a disease condition affects few or many people.”
Foundations have recently turned to a new kind of funding model: venture philanthropy. It works like a grant, except that instead of giving researchers money as if it were a gift, researchers are accountable to the funders. They get payments when they reach certain steps in the drug-development process. Also, those giving the money are doing so “in exchange for payments on later drug sales,” Hoffman says.
The model also recognizes the high failure rate of drug development. “If the drug fails at some point and things don’t work out, it just becomes a grant, so it’s forgivable,” he says.
Using venture philanthropy to fund the bulk of vamorolone’s development meant that Nagaraju and Hoffman didn’t give up any stock in ReveraGen BioPharma, the company they created. That meant they maintained control of it, removing any pressure for profit and keeping the focus on whom the drug should benefit: children with DMD.
“We often say our fiduciary duty is to the stakeholder, not stockholders,” Hoffman says.
It also means that they didn’t need to hype the drug before it was ready for clinical trials. That’s not always the case for drug development backed by venture capitalists, who want to make as big a splash as possible and may give overblown statements about what their drug could do. Hoffman and Nagaraju didn’t want to raise false hopes. “We’re quite comfortable being under the radar on purpose,” Hoffman says.
In total, developing vamorolone to this point has cost $55 million (that includes $25,000 in fees just for the name).
Hoffman says $55 million is less than the typical drug-development price tag, which can run into the hundreds of millions. Their funding model has also allowed them to “turn the crank and think outside of the box about doing things differently,” he adds.
For example, they asked the FDA to allow them to continue to provide vamorolone to patients who had finished a 2.5-year clinical trial if the patients wanted it (most did), instead of moving to traditional corticosteroids with all their side effects. But the drug would be given as part of a patient’s routine clinic visits — not within a clinical trial — even though vamorolone does not have final FDA approval. The FDA permitted the move under its Expanded Access Protocol (EAP), also known as compassionate use, which can allow a patient with a life-threatening condition access to an investigational drug. Soon after that decision, the FDA issued a press release saying other drug developers could consider asking for EAP for drugs showing promise, too.
“The foundations that aid [drug development] want you to take risks and they want you to move forward quickly with new technologies and new approaches,” Hoffman says.