Biomedical’s big year: Grants fund research on skin, heart cells, cancer and more
The Department of Biomedical Engineering has earned nearly $4 million in grants from 2018–20
The Thomas J. Watson School of Engineering and Applied Science’s Department of Biomedical Engineering has earned nearly $4 million in grants from 2018–20 (as of March 2020). Associate Professor Sha Jin alone received three grants totaling $1.2 million for her diabetes research. Funding agencies include the National Institutes of Health, the National Science Foundation and the National Institute of Standards and Technology.
GUY GERMAN
ASSOCIATE PROFESSOR
RESEARCH TOPIC: HUMAN SKIN
THE GOAL: Understanding how different factors can cause the mechanical properties of our skin to change. The human body has many barriers, and skin is arguably the most important, protecting us from the external environment. When skin becomes broken or ruptured, that barrier is lost. It can be caused by surgical incisions, penetrating trauma, diseases that cause lesions and chapping from cold environments. German explores how bacteria can degrade integrity; the effects of chronological- and photo-aging; and how to create bio-inspired materials that control crack propagation and the movement of fluids on their surfaces.
TRACY HOOKWAY
ASSISTANT PROFESSOR
RESEARCH TOPIC: HEART CELLS
THE GOAL: Turning stem cells into functioning cardiac cells.
The human heart does not have the ability to repair itself after heart attacks or similar cardiac events. By merging the fields of stem-cell biology, tissue engineering and cardiovascular physiology, Hookway is trying to make models of cardiovascular tissue in a Petri dish that are more similar to what is in our bodies. One challenge is that the heart is not one cell type; in fact, it is multiple types of cells working together to achieve function.
SHA JIN
ASSOCIATE PROFESSOR
RESEARCH TOPIC: DIABETES
THE GOAL: Generating pancreatic tissue from stem cells.
One experimental treatment for diabetes — currently in clinical trials through the U.S. Food and Drug Administration — is islet transplantation, but there are fewer donors than needed. Human-induced pluripotent stem cells — cells that can self-renew by dividing — could offer a renewable source for islets, but they remain a challenge because of limited knowledge about how islets form. Jin’s lab has been working to direct stem cells to differentiate and mature into pancreatic islet organoids using a variety of approaches; when successful, these islets would be transplanted into humans.
AHYEON KOH
ASSISTANT PROFESSOR
RESEARCH TOPIC: HUMAN SWEAT
THE GOAL: Utilizing sweat to generate electricity for flexible biosensors and to monitor stress levels.
Koh’s research aims to give us real-time information about how our bodies are functioning, such as for glucose monitoring, wound care and post-surgery cardiac health. She is currently working with other Binghamton professors on two microfluidic systems that can collect and use the sweat that our body produces. One of them will have sweat-eating bacteria that will power biosensors, and the other will monitor stress levels by measuring the amounts of the steroid hormone cortisol that are secreted.
GRETCHEN MAHLER
ASSOCIATE PROFESSOR
RESEARCH TOPIC: ORGAN-ON-A-CHIP
THE GOAL: Creating 3D microfluidic cell-culture chips that simulate the mechanics and physiological response of organs and tissues.
Mahler’s current research — which has applications for cardiovascular disease and cancer — focuses on how disruptions in a tissue’s mechanical or chemical environment can lead to disease initiation and progression. She currently is working with three other professors — two from Watson, one from Harpur College of Arts and Sciences — on a National Science Foundation-funded study of calcific aortic valve disease, and she also is interested in how food additives alter gastrointestinal health.
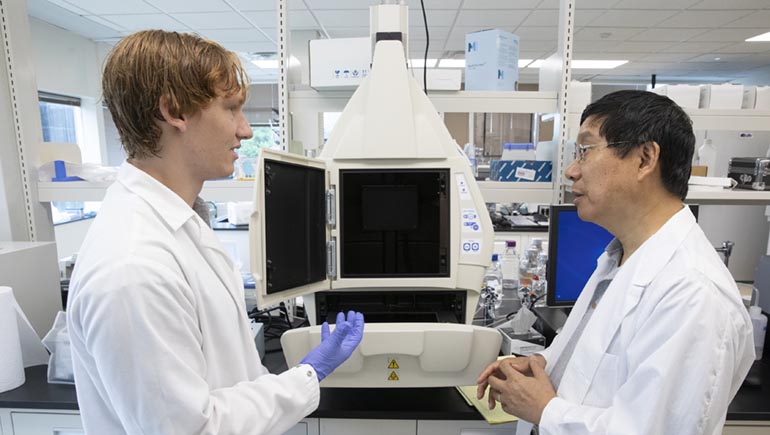
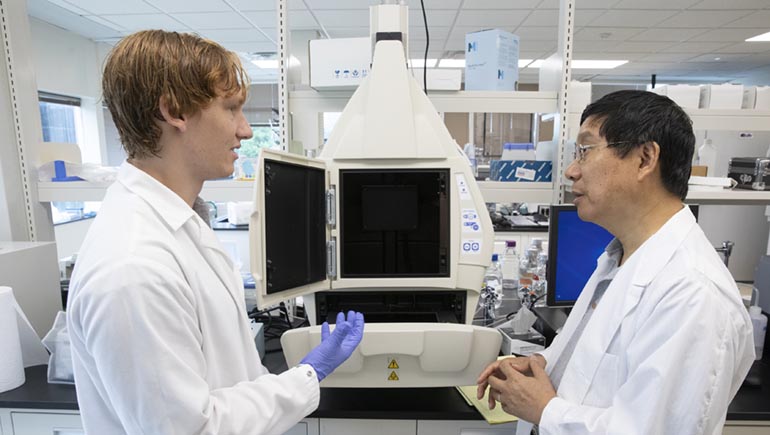
KAIMING YE
PROFESSOR AND DEPARTMENT CHAIR
RESEARCH TOPIC: CANCER VACCINE
THE GOAL: Developing a vaccine that will slow or halt the growth of future tumors.Ye’s research is targeting the protein CD47, which is part of the membrane that covers human cells. It also sends a “don’t eat me” signal to a body’s immune system — normally a good thing, but a problem when cells become cancerous. In a 2019 study using mice treated with their experimental vaccine, Ye and his co-investigators found a two-fold reduction in tumor growth rates and five-fold reduction in size in the tumors that did form.