Researchers from Watson College, Upstate Medical team up to study brain disease
The two schools' collaborations stem from a memorandum of understanding signed in 2022
The best partnerships are the ones where everyone benefits.
That’s why Upstate Medical University and Binghamton University’s Thomas J. Watson College of Engineering and Applied Science working together makes so much sense. Upstate Medical has research questions, and Watson can supply eager faculty and students as well as the technical equipment to help provide answers.
Since signing a memorandum of understanding in July 2022, the two schools have found ways to cooperate. Research areas being explored include neuroscience, brain imaging, digital pathology, cancer research and bone-tissue engineering. Under a pilot program that is part of the agreement, seed grants of up to $25,000 are awarded for preliminary research in pursuit of external funding. The two institutions also have submitted joint proposals to the National Science Foundation (NSF) and are exploring proposals to the National Institutes of Health (NIH).
One of those seed grants is funding a project led by Assistant Professor Fake “Frank” Lu from Watson’s Department of Biomedical Engineering and Dr. Satish Krishnamurthy, a professor of neurosurgery at Upstate Medical University. They are studying the underlying cause of hydrocephalus, a disorder where excess cerebrospinal fluid in the ventricles of the brain compresses brain tissue and causes a variety of physical and mental issues. It can happen to individuals at any age but is most common among babies and adults ages 60 and up.
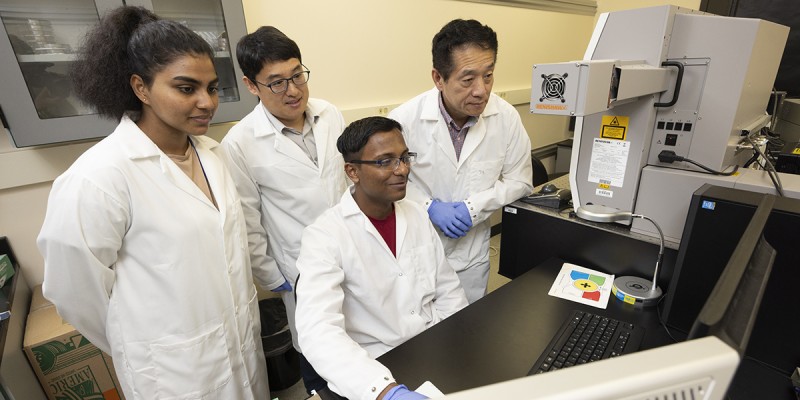
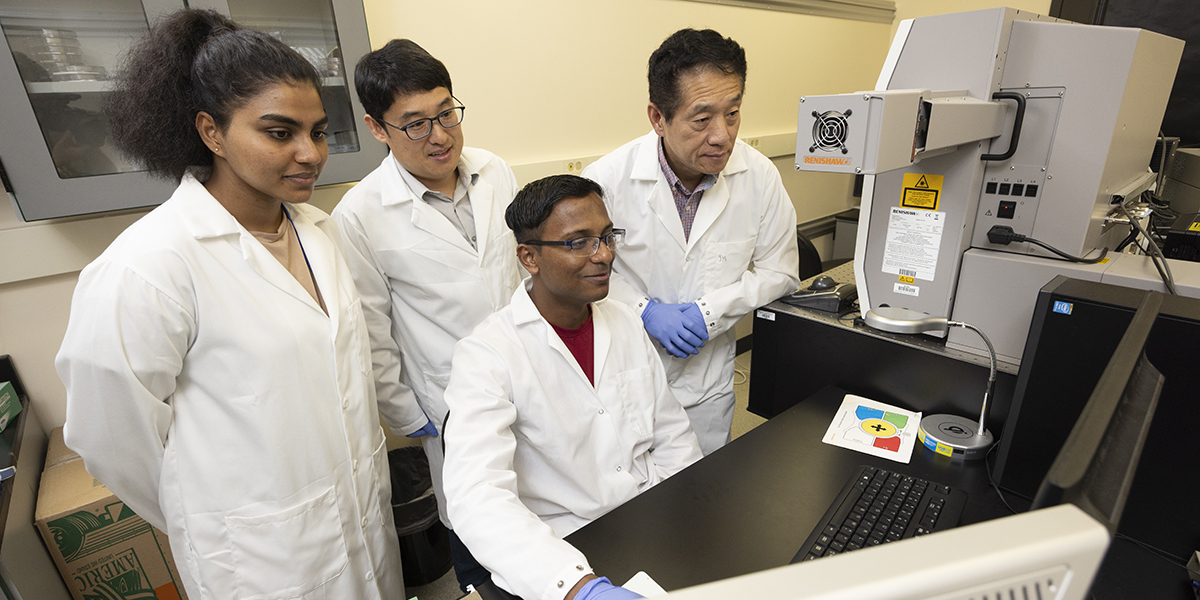
Over the summer, Upstate Medical research scientist Dr. Jie Li and Adithi Randeni, a British medical student from the University of Leeds, traveled to the biomedical labs at Binghamton’s Innovative Technologies Complex to work with Lu and PhD student Shovit Arpit Gupta. They analyzed how cerebrospinal fluid from hydrocephalus samples differs from normal samples using Raman spectroscopy, which uses scattered light to measure the vibrational energy modes of a sample and provide a structural fingerprint by which molecules can be identified.
“Our long-term plan is to develop an easy-to-use inline clinical setup to measure each patient very quickly, which will help us to understand their prognosis and make real-time decisions about surgical needs,” Lu says.
Because hydrocephalus is generally treated by installing a shunt that drains excess fluid away from the brain to lower in the body where it can be reabsorbed more easily, this research is to help understand the underlying process that causes hydrocephalus and treat it without surgery using medications.
“If the shunt malfunctions because of an infection or protein molecules blocking the port, the patient has to do a shunt revision or replacement,” Li says. “Currently, there’s no easy way to detect the shunt blockage, so that causes a lot of problems. I heard one kid had to go to the hospital for a shunt revision eight times in one year.”