A business-tech innovation for managing your medical records
Researchers show how to revive efforts to centralize data
Let’s say you have Type 2 Diabetes. For care, you go to your primary doctor and an endocrinologist. You may also see an eye doctor, nutritionist, podiatrist and exercise physiologist. That’s six providers, all of whom are responsible for your care — but are they sharing information?
The U.S. healthcare industry has failed to create an efficient and effective network for storing and sharing patients’ medical data, says Emre Demirezen, assistant professor of operations management at Binghamton University. The industry has also been slow to transition from paper to digital records. Health providers still store patient records in filing cabinets, fax lab results, and manually enter and transmit medical information.
“A patient’s medical history is often fragmented because people move from practitioner to practitioner, but their records don’t follow them,” Demirezen says. “Lack of coordination of care impacts both the patients and the providers in terms of time, money and health outcomes.”
Moving patient health records to a stream-lined electronic system has been a long-term goal of physicians, hospital administrators and policymakers. Federal money was first earmarked to establish systems to store and transfer medical data through healthcare information exchanges (HIEs) in 2009. Demirezen says HIEs allow clinical information (medical history, family medical history, medications prescribed, disabilities, allergies, etc.) to be transferred electronically among healthcare providers.
The benefits of HIEs may be obvious to proponents, but problems related to cost, implementation and vitality have been little explored by experts, says Demirezen, who co-authored a paper on the topic with professors Subodha Kumar and Arun Sen of Texas A&M University.Their paper, “Sustainability of Healthcare Information Exchanges: A Game–Theoretic Approach,” was featured in Information Systems Research — one of the top three journals in management information systems — in June 2016.
The paper states, “HIEs will reduce duplication of tests; paper, ink and manual document printing needs; and phone calls and other follow-ups for test results.” But Demirezen says the vitality of HIEs continues to be called into question because they rely heavily on federal funding but do not have bipartisan support.
“We illustrate strategies to help the HIEs survive in the long run,” Kumar says. “Our paper is the first to examine how to holistically optimize your HIE network. Previous research focuses only on the policymaker or the HIE administrator side of the operation.”
“If the implementation and facilitation of HIE is done incorrectly, the exchange services will not survive,” adds co-author Sen. “We study how an HIE can be sustained financially by developing cost structures for the providers participating in the HIEs.”
Their research also suggests ways for healthcare administrators and policymakers to encourage more providers to implement and use HIEs. “We explore strategies for HIEs to stay financially viable and not need government spending or policymaking to continue,” Demirezen adds.
By examining current data-exchange trends, the researchers outline best practices in terms of implementing HIEs in regions under different conditions. In regions where heterogeneity among health providers is high, with the presence of both large and small health practices, there are several strategies to increase HIE participation:
Financial incentives
Financial incentives are one way to encourage hospitals and practitioners to use technology to log and transfer patient medical data. The paper suggests that HIE providers, whether public or private, should offer more incentives to help small health providers establish electronic health-record systems at a very low cost or for free.
Demirezen says that basic incentives alone will not entice all health providers to join a network, especially when there are both large and small providers in the region.
Enhancing value
Another way to increase participation in these exchanges is by offering more features, or value-added services, in addition to basic connectivity to an HIE. Examples of value-added services could be the use of an e-prescription tool or quality management portals.
“Value-added services are one of the best possible business strategies for sustaining HIEs,” Demirezen says.
Multiple networks
Demirezen also suggests that adding a second network in a region could increase the HIE participation among low-gain providers, or providers that will expect a low gain in terms of profit and value after joining an HIE.
“We found that having a second HIE in the same region that only focuses on low-gain providers could cause more providers to participate in the exchange,” he says. “Our research also suggests that certain providers would be more interested in participating in an HIE if the second HIE promises more value to them, such as offering electronic health record solutions for free or at a discount.”
Data-driven future of healthcare
Kumar says HIEs are “still really abysmal in terms of their efficiency and ability to exchange information.” However, he believes there will be a strong momentum to increase adoption by providers, improve participation levels and maximize interoperability.
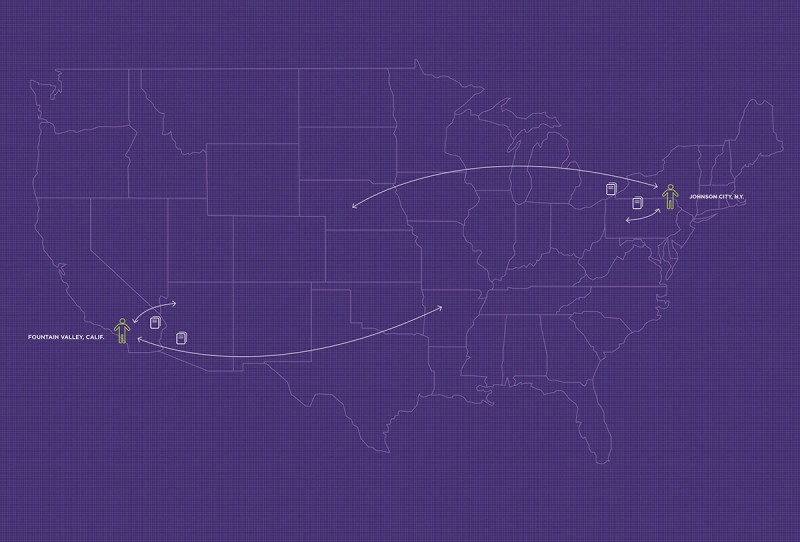
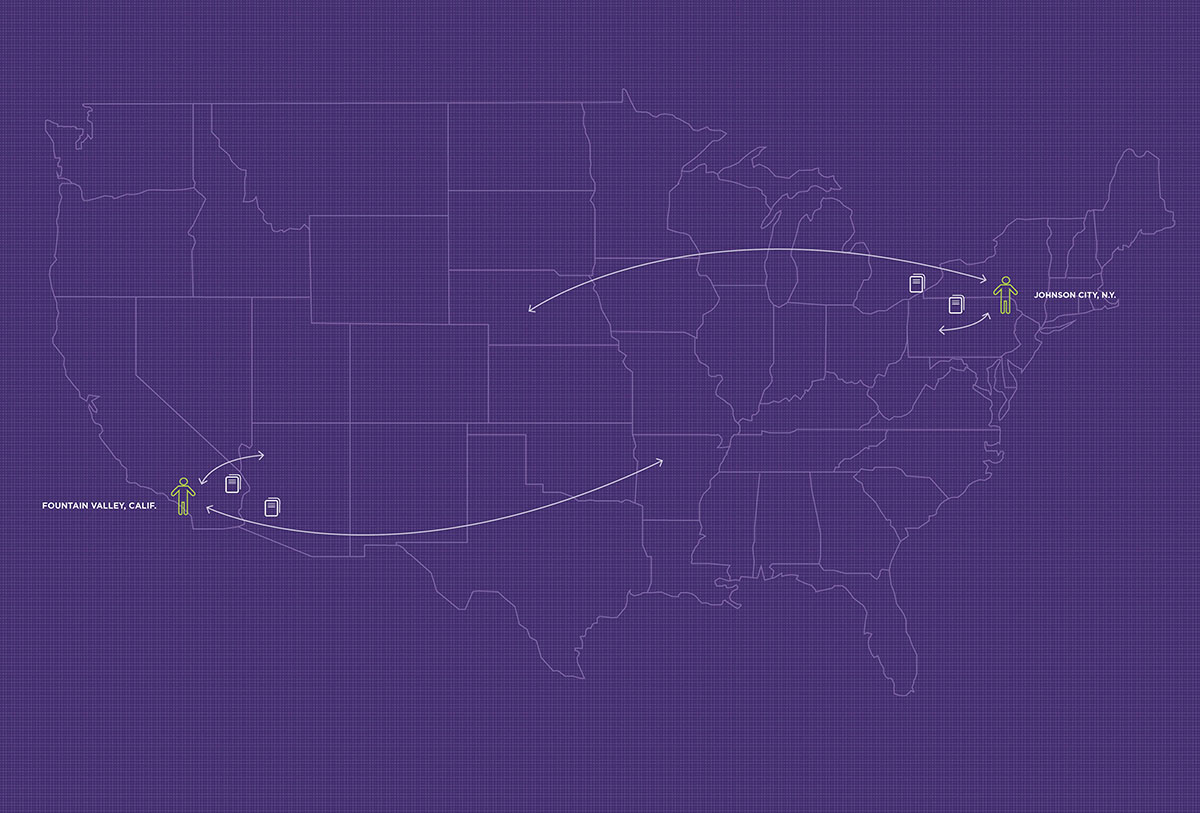
“The healthcare industry is moving toward a trend where one provider is connected to multiple healthcare information exchanges. Twenty or so years down the road, all healthcare providers in the United States will be exchanging information. So if you live in New York but become hospitalized in California, there won’t be an issue sending your medical information across the country,” Kumar says.
“There’s no question whether or not HIEs will improve the healthcare system. Now, it’s a matter of how the industry can make these exchanges financially viable and sustainable,” Demirezen adds. “The big idea is to eventually have all of the HIEs interconnected. Wider use of the automated transfer of electronic health records can help control costs and ensure there are fewer errors in medical care.”
In 2016, Demirezen published three papers in top-tier journals. He has presented the HIE sustainability research at several international conferences. Demirezen is supply chains because of their high potential to impact academics and real life.
“I research whatever topic interests me at the moment. But with healthcare, I also feel like I am making a real difference — assisting people in getting more efficient and effective care goes beyond business,” he says.
Demirezen is working with HealthLinkNY, a Binghamton-based healthcare information exchange provider, to explore new research focusing on the benefits of HIEs. In particular, he will explore how these networks can reduce a patient’s length of stay and the likelihood for readmission through the emergency room.
“To deliver affordable, high-quality and efficient care, a physician or hospital needs the ability to obtain and transfer good information. HIE leverages technology to provide a continuum of care that is necessary to innovate the industry,” Demirezen says.