New Binghamton University clinical program aims to improve rural healthcare
$1.2 million HRSA grant funds NP training, preceptor support

Binghamton University’s Decker School of Nursing is using HRSA funding to launch a program aimed at keeping rural advanced practice nurses in rural communities.
“Rural healthcare organizations invest a lot of resources recruiting healthcare providers, who often leave after only a year or two because they don’t like living in a rural area,” says Nicole Rouhana, director of graduate programs at Binghamton University’s Decker School of Nursing. “This leaves many rural communities without adequate access to primary care providers and services.”
This fall, the Decker School is launching a new clinical training program that aims to change that by starting with students who already live in a rural area.
“We have identified 14 family care nurse practitioner students who are from areas with a designated rural status of 4 or more [as defined by the locale’s United States Department of Agriculture rural-urban community area code] and are matching them with rural sites that are located in the students’ community. The student will complete all 660 clinical hours of direct, supervised patient care in one rural site,” Rouhana says. “We believe this extended clinical placement will foster an incredibly strong connection between the student and the hosting clinical site and may result in long-term employment, which benefits both the student and the rural community.”
The program is being funded by a $1.2 million grant from the Health Resources and Services Administration’s (HRSA) Advanced Nursing Education Workforce (ANEW) Program.
“The ANEW grant is designed to offer one solution to the issue of providing a well-educated, advanced-practice nursing workforce in rural communities,” says Pamela Stewart Fahs, associate dean, director of doctoral programs and the Decker Chair in Rural Health at Binghamton University. “The program provides a means to educate advanced-practice nurses in a manner that keeps them engaged in the rural community as they learn and will position them to be part of the workforce solution for rural healthcare after they graduate.”
In addition to tuition assistance, the HRSA funding is being used to provide the NP students with advanced technology and a variety of clinical tools and software that will introduce them to the foundations of telehealth.
“This funding helps me pay for a large part of my graduate school tuition,” says Kathryn DeWitt, second-year FNP student from Susquehanna, Pa. “Being a part of this program means that I will be able to uphold a high standard of care in my rural hometown.”
“This grant has given me the opportunity to make a positive impact on the rural health community and specifically, in my hometown rural community,” says Beth Plumadore, first-year FNP student from Saranac, N.Y. “Growing up in a rural area, I have firsthand experience with lack of healthcare in this setting. Many people in my home community have to travel long distances to receive medical care or choose not to receive care at all due to inaccessibility and inconvenience.”
The HRSA grant is also funding the purchase of telehealth equipment for the clinical sites.
Rouhana, who co-authored the grant with Fahs, explains that the provision of telehealth equipment at clinical sites where the students are being placed is an important part of the project. It not only enables Binghamton instructors to connect with students regularly without requiring on-site visits, but also provides continuing-education opportunities to clinical preceptors in these locations. Additionally, providers — who will be trained on the use of the equipment by Binghamton telehealth expert Ann Fronzcek, assistant professor or nursing — will be able to use the equipment within their organizations.
“One of our program goals is to support our clinical preceptors in these rural areas by providing them with tools and training to use telehealth to enhance the care they provide to their patients,” says Rouhana.
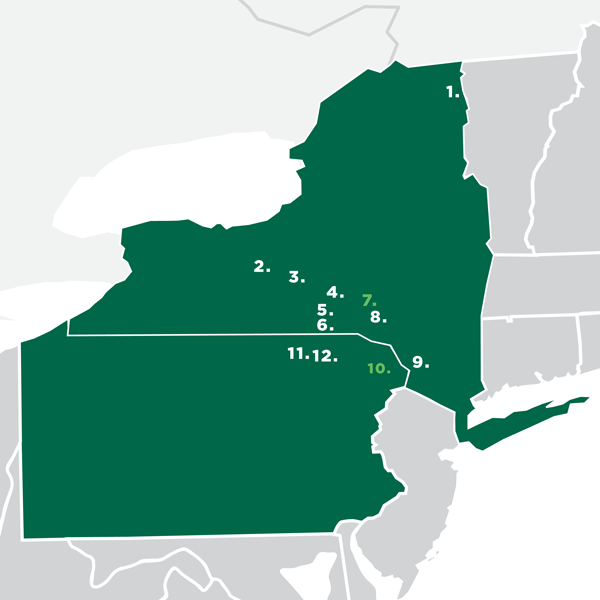
Over the course of two years, first- and second-year students from 12 rural locations in New York and Pennsylvania will receive funding and support through the program.
“It is crucial to increase the number of rural healthcare providers because rural communities are severely underserved,” says DeWitt. “The HRSA grant program will help attract quality practitioners to these areas.”
“By working in the rural health setting, I have the opportunity to improve healthcare for these people and provide care for the community,” says Plumadore. “My ultimate goal is to work in my home community in rural upstate New York to make a positive difference for those I was raised with. The HRSA grant has given me a new outlook on healthcare and made me realize the impact I can make as a provider.”
This marks the second grant the Decker School has received from HRSA. In July 2016, Decker was granted $350,000 to support training for advanced-practice registered nurses who are from underrepresented minorities or have veteran status. This one-year grant fully funded 20 students.