The missing link: pancreatic polypeptide
Researchers at Binghamton University have created insulin-secreting pancreatic islet tissues that are bringing scientists closer to a cure for diabetes.

Researchers from the Biomedical Engineering Department at Binghamton University have generated insulin-secreting islet tissues with a composition that matches pancreatic islets. The new development could be an important step for long-term diabetes treatment.
As of 2017, the Centers for Disease Control and Prevention (CDC) reported that more than 100 million Americans currently have diabetes or prediabetes. This number has been rapidly growing over the past few years.
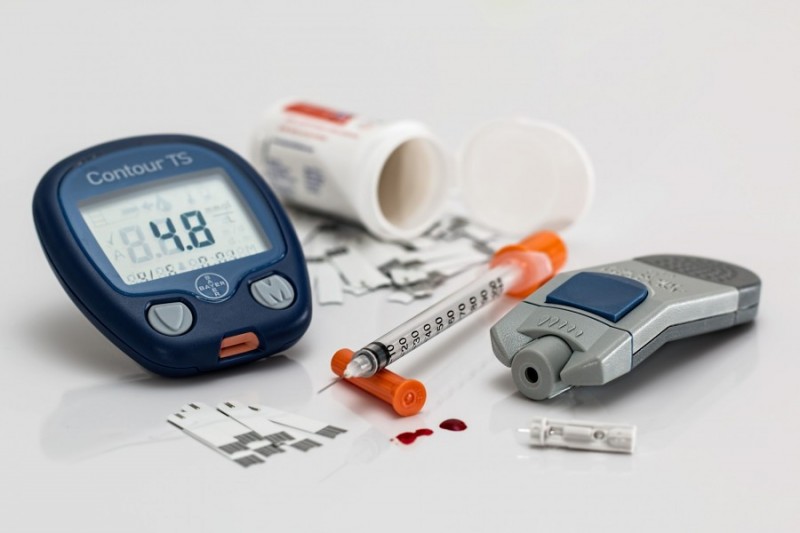
Since there is currently no cure for diabetes, those diagnosed with the disease are only able to manage it with a combination of medication, such as insulin injections that might be administered multiple times every day, and general lifestyle adjustments.
Associate professor Sha Jin and professor Kaiming Ye from Binghamton University worked on the study with Weiwei Wang from the University of Arkansas. Their research aimed to find a way to actually replace the diabetic cells with non-diabetic ones.
“When patients have diabetes, that means that the cells in their pancreas don’t produce enough insulin or the body doesn’t respond to the insulin well,” said Jin.
Insulin injections are a way to compensate for those deficiencies but researchers have been searching for a way to cure diabetes at the source.
“Scientists have been working on creating insulin-secreting beta cells, but until our study no one has been able to create insulin-secreting islets that include pancreatic polypeptide [PP] cells,” explained Jin.
A pancreatic islet consists of glucagon-secreting alpha cells, insulin-secreting beta cells, somatostatin-secreting delta cells and pancreatic polypeptide-secreting PP cells. This composition is crucial for controlling glucose metabolism. While pancreatic polypeptide makes up approximately one percent of pancreatic islets, it still plays a role in pancreatic secretion activities.
“The lab-produced islets can be used for the disease models of diabetes-related pathophysiology, for drug testing and for islet transplantation that could lead to a cure for diabetes,” said Jin. “We used human embryonic stem cells in biomimetic 3-D scaffolds to develop these islet tissues.”
In the past, stem cell research has raised ethical issues about our definition of personhood, but a key change rids stem cell research of these ethical quandaries.
That’s because around 2009, stem cell research started to change what was meant by human embryonic stem cells.
“We now use stem cells that come from a person’s own skin cells. This helps us by avoiding the potential ethical issues associated with using an embryo,” said Jin.
These skin stem cells could have additional benefits for any patients seeking transplants.
“Instead of relying on organ donations, which are scarce, we may be able to build an organ from someone’s own stem cells. This means the body will be less likely to reject the transplant,” explained Jin.
According to the United Network for Organ Sharing (UNOS), someone is added to the national transplant waiting list every 10 minutes and about 20 people die every day waiting for a transplant.
However, Jin made sure to point out that this study is only one part of the story for a diabetes cure.
“Type I diabetes is an autoimmune disease. We can replace the pancreatic cells with healthy ones, but we also have to find a way to protect those cells from the body’s immune system,” she says.
Jin explained that there are currently other researchers working on this problem who hope to create a type of shield for the insulin-secreting cells.
Once the kinks are ironed out, the idea is that diabetes could become curable through a pancreas transplant using islets derived from a patient’s own skin cells.
The study, titled “Development of Islet Organoids from H9 Human Embryonic Stem Cells in Biomimetic 3D Scaffolds,” was published in Stem Cells and Development.